Local news outlets are full of reports that are startlingly similar: drug overdose deaths are spiking. But with the pandemic dominating the headlines and crowding out much of the health news, it’s easy to have missed the CDC’s Provisional Drug Overdose Death Counts report issued earlier this month that raised the alarm about more than 80,000 drug overdose deaths in 2020, a more than 20% spike over the prior year. As if the year weren’t a nightmare enough with Covid-19-related deaths, it was also was the year with the highest number of overdose deaths ever recorded in a single year.
Usha Lee McFarling reports for Stat News: As the pandemic ushered in isolation and financial hardship, overdose deaths reached new heights, saying that much of this increase is the result of a perfect storm – stress, isolation and economic upheaval, all triggers for addiction and relapse. To make matters worse, many of the usual social support networks that people rely on for support are inaccessible during the pandemic. She cites isolation as a major contributing factor, affording those using opioids, alcohol, and other substances in secrecy.
“The increase in opioid deaths is crushing to those who work in public health and addiction treatment, who were finally making headway, thanks to growing public attention and government funding. Overdose deaths had fallen in 2018 for the first time in years. But the spread of fentanyl began to erode those gains, and now the pandemic has severely undercut efforts to control the opioid epidemic; with public health officials focused so heavily on the coronavirus, suffering and death due to substance abuse has largely fallen off the radar.”
Covid-19 is not only robbing much of the time and attention that healthcare workers might otherwise focus on addiction, McFarling says that, “the financial toll of the pandemic means many cash-strapped health care systems are cutting addiction treatment programs just when they are needed most.”
Valerie Bauman and Ian Lopez have also reported on this issue in Bloomberg Businessweek: The Opioid Crisis, Fueled by Covid, Is Worse Than Ever, noting that opioids accounted for more than 61,000, or 73%, of last year’s deaths. They say:
“The opioid epidemic has been eclipsed in the public consciousness by Covid-19, but it hasn’t abated. The pandemic has only exacerbated the crisis, piling stress and grief on top of substance-abuse problems and jeopardizing efforts at recovery.”
The US Surgeon General has previously declared the opioid crisis a nationwide Public Health Emergency. In November 2016, the Office of the Surgeon General released Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health (the Surgeon General’s Report), noting that only about 10 percent of people with a substance use disorder receive any type of specialty treatment. This treatment gap leaves an estimated 90% of people with substance use disorder who go untreated.
What can employers do?
Employers suffer the economic costs of the nation’s opioid problems in absenteeism, lost productivity, workplace accidents, and more. Employers have a unique opportunity to help address this crisis because they are often able to spot substance abuse problems early in deteriorating work performance or diminished productivity. The leverage of a job and associated income means that employers hold the potential to play a key role in early intervention in helping an employee to seek treatment.
Some of the ways employers can help include:
- Implementing substance-free workplace programs
- Developing and promote policies about workplace drug and alcohol use
- Providing drug and alcohol awareness training to managers and the workforce at large
- Implementing drug testing programs – particularly important for employees with safety sensitive roles
- De-stigmatizing mental health and substance abuse issues by providing education
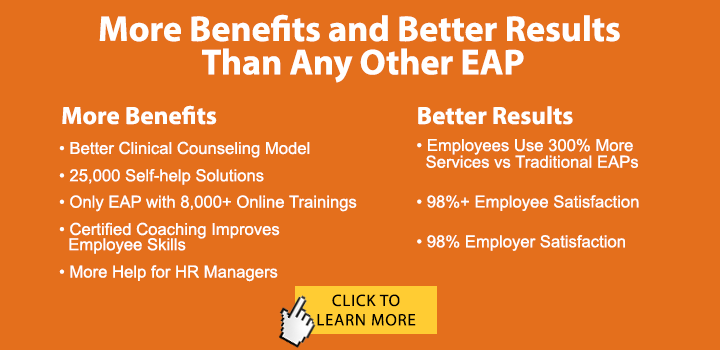
- Promoting available help resources such as the EAP and community or health-plan related health and wellness programs
- Working in tandem with an EAP benefit, which trains supervisors and managers in referrals
Today, the prevalence of remote work during the pandemic makes it more difficult for supervisors and employers to observe and detect a deterioration in work performance, which is frequently a sign that the employee is experiencing some life disruption. Deteriorating work performance can be related to a number of issues: substance abuse, family problems, a health crisis, depression, or many other issues. Sometimes, alcohol or substance abuse is fairly evident, but it is not an employer’s job to diagnose. Rather, performance deterioration is often an appropriate entry point to an Employee Assistance Program (EAP), where experienced counselors can help to assess the root cause of the problem and refer the employee for the appropriate help.
Your employee assistance program should be an integral component of your drug treatment programs. At ESI EAP, we offer a complete Drug Free Workplace and DOT Compliance Program, including substance abuse education and prevention, as well as counseling and coaching for substance abuse and addiction and referrals to inpatient treatment programs, when needed. We also offer DOT compliant training for safety-sensitive workers. ESI EAP has been dealing with work-related substance abuse issues for more than 30 years.